Background: Current risk stratification for primary gastrointestinal diffuse large B-cell lymphoma(PGI-DLBCL) relies on mainly on clinical factors. Radiomics score (RadScore) associated with survival outcomes have been developed for other cancer types, however few studies have thus far examined the role of radiomics in PGI-DLBCL.
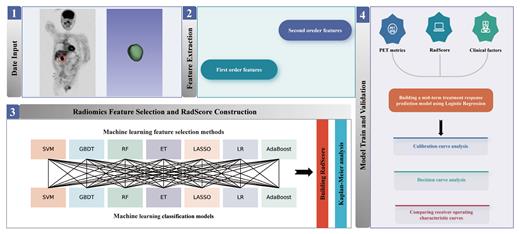
Objective: In this study, we investigated the value of PET RadScore constructed using a machine learning cross-combination approach in predicting the early treatment response and prognosis of patients with primary gastrointestinal diffuse large B-cell lymphoma (PGI-DLBCL) treated with the R-CHOP-like regimen.
Methods: A retrospective analysis was conducted on 108 PGI-DLBCL patients diagnosed through histopathological examination at two independent medical centers from March 2011 to March 2023, with 86 patients in the training cohort and 22 patients in the validation cohort. Seven different machine learning models were used to generate 49 feature selection-classification candidates, and the optimal candidate was selected based on the area under curve of ROC to establish RadScore. Risk factors were identified through logistic regression, and a radiomics nomogram was constructed by combining RadScore with the selected risk factors. The model was evaluated through calibration curves and decision curve analysis (DCA) using the training cohort and validation cohort.
Results:A total of 111 radiomics features were extracted, and 19 features with strong predictive performance were selected to generate RadScore. The results suggest that RadScore can stratify patient prognosis.The logistic regression analysis results in the training cohort showed that elevated lactate dehydrogenase (LDH) level (OR=3.53, 95%CI: 1.21-10.31, p=0.021), intestinal involvement (OR=3.04, 95%CI: 1.04-8.88, p=0.042), and total lesion glycolysis (TLG) (OR=6.73, 95%CI: 2.23-20.29, p<0.001) were independent risk factors for predicting early treatment response. A multi-parameter model incorporating clinical risk factors, metabolic factors, and RadScore was constructed (training cohort AUC: 0.834; validation cohort AUC: 0.902), and the performance of the model was evaluated.
Conclusion:The RadScore, constructed based on a cross-combination approach using machine learning, can predict the survival of PGI-DLBCL patients. When RadScore is combined with clinical risk factors and metabolic factors, it forms a combinatorial model suitable for predicting early treatment response to R-CHOP-like chemotherapy regimens. Larger studies will be needed to validate these results.
Keywords : Primary gastrointestinal diffuse large B-cell lymphoma · [18F]FDG PET/CT · Early treatment response · Prognosis · Machine learning
Disclosures
No relevant conflicts of interest to declare.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal